Antihistamine Effectiveness & Drowsiness Comparator
Select your priority to see which antihistamine best matches your needs. Based on clinical data from the article.
Cetirizine (Zyrtec)
Fast-acting (30 min), best for severe itching
Max dose: 20mg/day (safe up to 40mg)
Loratadine (Claritin)
Mild to moderate relief, good for sensitive users
Max dose: 10mg/day
Fexofenadine (Allegra)
Slow-acting (2.5 hrs), best for focus-sensitive users
Max dose: 180mg/day
Your Recommendation
Select your priority above to see your recommendation.
Important Safety Notes
• Never combine two first-generation antihistamines (e.g., Benadryl + hydroxyzine)
• Doses above 40mg cetirizine carry rare QT prolongation risk
• Always consult your doctor before increasing doses
• Heart conditions may require special monitoring
When hives show up - those sudden, itchy, raised welts on your skin - you want relief, fast. Most people reach for an antihistamine first. But not all antihistamines are the same. Some knock you out. Others barely touch the itching. And if they stop working after a few weeks, you’re left wondering: what now?
How Antihistamines Actually Work on Hives
Hives aren’t just a rash. They’re your body’s allergic reaction turned up too loud. Mast cells in your skin release histamine - a chemical that makes blood vessels leak fluid into surrounding tissue. That’s what causes the swelling, redness, and itch. Antihistamines block the H1 receptors that histamine binds to, stopping the signal before it turns into a flare-up.
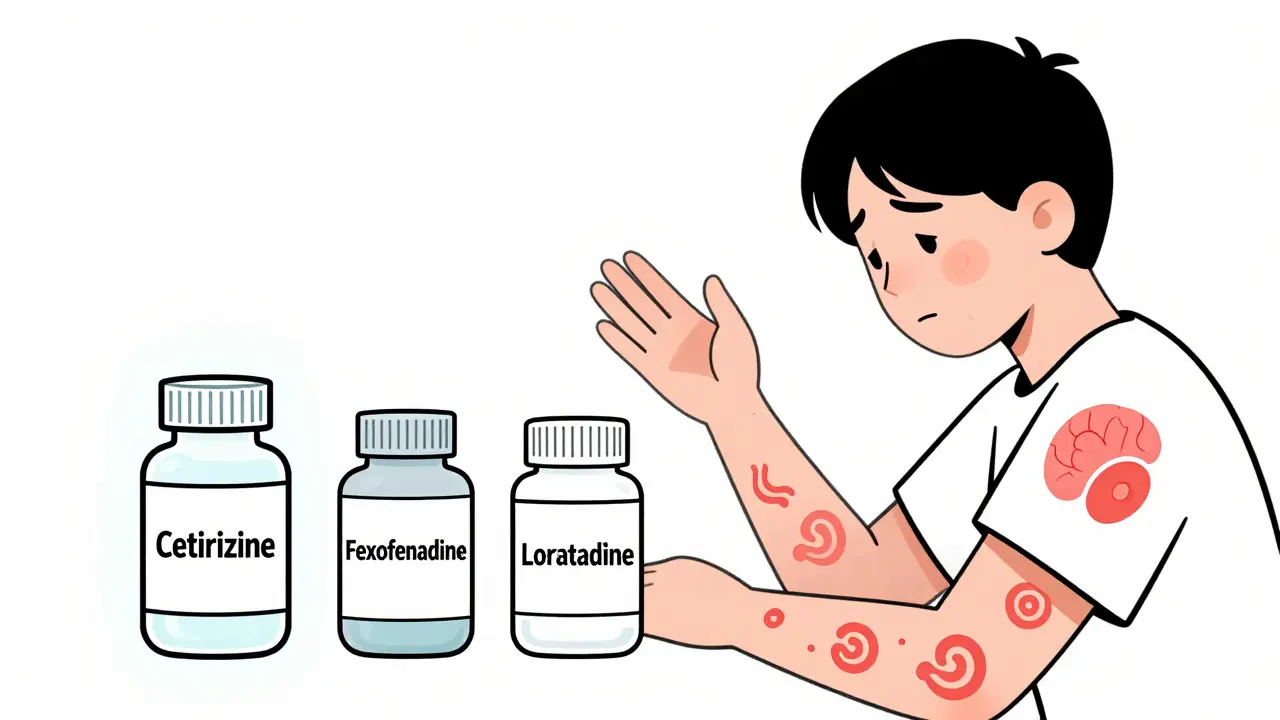
There are two main types: first-generation and second-generation. First-gen drugs like diphenhydramine (Benadryl) were developed in the 1940s. They work fast - often within 30 minutes - but they cross into your brain easily. That’s why half of people who take them feel drowsy, sluggish, or foggy. Second-gen antihistamines like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) were designed differently. Their molecules are bulkier, so they can’t slip through the blood-brain barrier as easily. That’s why they’re called non-sedating.
Why Drowsiness Isn’t Just a Side Effect - It’s a Dealbreaker
Many assume drowsiness is just an annoyance. But for people with chronic hives, it’s a daily burden. You can’t afford to nod off at work, drive your kids to school, or focus on a meeting. Studies show 50% of people taking Benadryl report drowsiness. Even second-gen options aren’t perfect. About 10-15% of users still feel tired, especially with higher doses.
Here’s the real difference:
- Cetirizine (Zyrtec): 10mg daily works for most. But 38% of users report drowsiness - higher than other second-gen options. It’s the most effective for itching, but the trade-off is real.
- Loratadine (Claritin): Less potent than cetirizine, but only 12% report drowsiness. Good for mild cases or if you’re sensitive to side effects.
- Fexofenadine (Allegra): Lowest drowsiness rate at 22%. Takes longer to kick in - about 2.5 hours - but you’re less likely to feel foggy. Best for people who need to stay sharp.
A 2021 study tracking 342 people with chronic hives found cetirizine reduced itching by 78%, while fexofenadine only cut it by 65%. But in driving simulations, fexofenadine users showed 8% cognitive impairment - half the rate of cetirizine users. If your job demands focus, fexofenadine might be the smarter pick, even if it’s slightly less effective.
What If Your Antihistamine Stops Working?
It’s not uncommon. About 57% of people with chronic hives don’t get full relief from standard doses. Some notice it after a few weeks. Others feel it creep in over months. Reddit’s r/urticaria community has over 14,000 members - and 68% say their original dose stopped working within six months.
The fix isn’t always switching brands. The first step is increasing the dose. Guidelines now say it’s safe to go up to four times the normal dose. That means 40mg of cetirizine daily, not 10mg. This works for about 30% of people who didn’t respond to standard doses. A 2022 review of 12 trials confirmed this approach boosts control rates from 43% to 73%.
But here’s the catch: higher doses aren’t risk-free. The FDA has noted rare cases of QT prolongation - a heart rhythm issue - at doses above 40mg. It’s uncommon (0.2% of users), but if you have heart problems, kidney disease, or take other meds that affect your heart, talk to your doctor before escalating.
Alternatives When Antihistamines Just Don’t Cut It
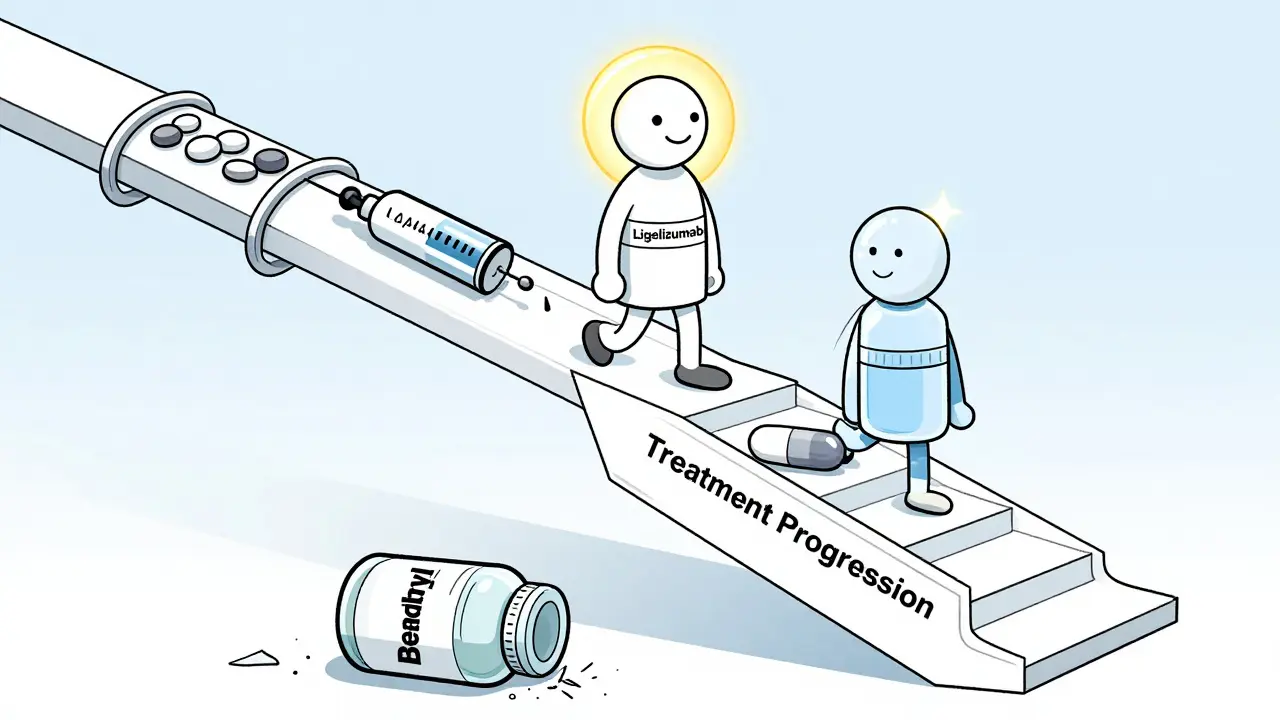
If doubling or quadrupling your dose still leaves you covered in hives, it’s time for the next tier of treatment. These aren’t backup options - they’re proven solutions for people who’ve tried everything else.
- Omalizumab (Xolair): This is an injectable biologic approved specifically for chronic hives that don’t respond to antihistamines. It targets IgE, the antibody that triggers mast cells. In trials, 58% of patients got complete relief. It’s given once a month. The downside? It costs around $3,200 per shot. Insurance often covers it if you’ve tried high-dose antihistamines first.
- Ligelizumab: The new kid on the block. In phase 2 trials, it showed a 51% complete response rate - better than omalizumab’s 26%. The FDA gave it Breakthrough Therapy status in March 2023. Phase 3 trials are wrapping up in mid-2025. If approved, it could become the new gold standard.
- Cyclosporine: An immune suppressant used for severe cases. It works in about 65% of patients. But it can damage your kidneys over time. Only used short-term, under close monitoring.
- Leukotriene blockers (like montelukast): Sometimes added to antihistamines. Not as powerful alone, but can help a little extra - especially if you also have asthma or nasal allergies.
One study ranked treatments by effectiveness. Omalizumab scored 98.7 out of 100. Ligelizumab came in at 94.3. Cyclosporine at 85.2. High-dose antihistamines? Only 62.1. The gap is real.
How to Track What’s Working - and What’s Not
Guessing doesn’t help. Tracking does.
Use a daily symptom diary. Note:
- Number of hives (count them)
- Intensity of itching (1-10 scale)
- Medication taken and time
- Any possible triggers: stress, heat, NSAIDs like ibuprofen, tight clothing, alcohol
The Urticaria Activity Score is the gold standard doctors use. But you don’t need a medical form. A simple notebook or the Hive Wise app (rated 4.2 on the App Store) works fine. People who tracked for just 4 weeks found triggers they never noticed - like heat from showers or a new laundry detergent. One user found 32% of flare-ups happened after taking Advil. Stopping it cut her flares in half.
When to See a Specialist
Most primary care doctors start you on antihistamines. But only 32% feel confident handling cases that don’t respond. That’s why 68% of patients end up referred to an allergist or dermatologist.
You should see a specialist if:
- You’ve tried four times the standard dose for 4+ weeks with no improvement
- You’re having hives every day for more than 6 weeks
- You’re experiencing swelling in your throat, tongue, or lips (this could be angioedema - a medical emergency)
- You have other autoimmune conditions like thyroid disease - people with these are 3.2x more likely to have treatment-resistant hives
Specialists can order blood tests. High-sensitivity C-reactive protein (hs-CRP) levels above 3mg/L predict a 78% chance you won’t respond to antihistamines. That’s not just a number - it’s a roadmap to your next step.
What’s Coming Next
The future of hives treatment is getting personal. Researchers are looking at:
- Pharmacogenetics: Some people metabolize cetirizine slower due to a gene variant (CYP2C19). Testing for this could tell you if you need a higher dose - or a different drug.
- New mast cell stabilizers: Seven compounds are in clinical trials. These aim to stop mast cells from releasing histamine in the first place - without the side effects of immunosuppressants.
- Better biologics: Ligelizumab could be approved by late 2025. Others are in the pipeline. The goal? More effective, less expensive, and easier to take.
But here’s the truth: antihistamines aren’t going away. They’re still the first step because they’re safe, cheap (generic cetirizine costs $15/month), and work for nearly half of all patients. The goal isn’t to replace them - it’s to use them smarter, and know when to move on.
Final Takeaways
- Start with a second-generation antihistamine - cetirizine, loratadine, or fexofenadine. Avoid Benadryl unless it’s a one-time emergency.
- If it doesn’t work, don’t switch brands - increase the dose. Up to 40mg of cetirizine daily is safe for most.
- Track your symptoms daily. Triggers like stress, heat, or NSAIDs are often the hidden cause.
- If you’re still breaking out after 4 weeks of high-dose antihistamines, see a specialist. You may need a biologic like Xolair or soon, ligelizumab.
- Don’t wait until hives control your life. Effective treatments exist - you just need to know the right path.
Can I take two different antihistamines together for hives?
Yes - and it’s often recommended. Combining cetirizine and fexofenadine is a common strategy when one drug alone isn’t enough. Studies show this combo improves symptom control without increasing drowsiness. But never combine two first-generation antihistamines like Benadryl and hydroxyzine - that raises the risk of dangerous side effects.
Is there a non-pill option for antihistamines?
Yes. Cetirizine and loratadine come in liquid, chewable, and dissolving tablet forms. For people who have trouble swallowing pills, these are just as effective. Topical antihistamine creams (like diphenhydramine lotion) are not recommended for hives - they don’t penetrate deep enough to help, and can even cause skin irritation.
Do antihistamines cure hives?
No. They suppress symptoms by blocking histamine, but they don’t fix the root cause. Chronic hives often resolve on their own within months to years. The goal of treatment is to control symptoms until your body calms down. That’s why you keep taking them daily - even when you feel fine.
Can stress cause hives to get worse?
Absolutely. Stress doesn’t cause hives, but it triggers flare-ups in about 28% of chronic sufferers. Your body releases cortisol and adrenaline under stress - which can activate mast cells. Managing stress with sleep, exercise, or mindfulness can reduce frequency and severity. It’s not a cure, but it’s one of the most effective low-cost tools you have.
Are natural remedies like quercetin or vitamin C helpful for hives?
There’s no strong evidence that supplements like quercetin, vitamin C, or omega-3s reliably control hives. Some people swear by them, but clinical trials haven’t shown consistent results. Don’t skip proven treatments in favor of unproven ones. If you want to try supplements, talk to your doctor first - some can interact with medications.
How long should I take antihistamines for hives?
For acute hives (lasting less than 6 weeks), take them until symptoms are gone - usually a few days to a week. For chronic hives, guidelines recommend daily use for at least 3-6 months, even if you’re symptom-free. Stopping too soon often leads to rebound flares. Only stop under a doctor’s guidance.




Sarah Williams
The data on cetirizine vs. fexofenadine is solid, but nobody talks about the real issue: pharmaceutical companies design sedating antihistamines to keep people dependent. If they made a truly non-sedating option that worked better, profits would drop. This isn’t medicine-it’s corporate engineering.
Christina Weber
You misspelled 'fexofenadine' in your first paragraph. Also, 'drowsiness isn't just a side effect-it's a dealbreaker' is grammatically incorrect. The dash should be an em dash, not an en dash. And 'it's' is a contraction for 'it is,' not the possessive. Please proofread before posting. This isn't Twitter.
Cara C
I’ve been on 40mg of cetirizine for 8 months now. It’s not perfect, but I can finally sleep through the night. The key is tracking-started a simple Google Sheet with itch scores and triggers. Turns out, my laundry detergent was the culprit. No magic pill, just small changes adding up.
Michael Ochieng
As someone who moved from India to the US, I’ve seen how differently hives are treated here. Back home, people rely on Ayurvedic herbs and avoid meds unless absolutely necessary. But honestly? After my flare-up lasted 11 weeks, I’m glad I found this guide. The dose-escalation advice saved me.
Jerry Peterson
Just wanted to say thanks for laying this out so clearly. I’ve been avoiding doctors because I didn’t want to be told to ‘just take Benadryl.’ This feels like the first real roadmap I’ve seen. Even the part about stress-yeah, I didn’t realize how much my job was making it worse.
Sandy Crux
Of course, the article ignores the fact that all antihistamines are just Band-Aids-because the real cause? Glyphosate in our food supply. The FDA knows this. They’ve suppressed studies linking histamine overload to Roundup exposure. You’re being sold a lie. Xolair? It’s just another profit-driven distraction from the truth.
Hannah Taylor
wait so u mean to say we shud just take more zyrtec?? like 4x?? but what if u get weird heart palpitations?? i think the big pharma is hiding this bc they want ppl to buy xolair which costs 3k a shot lol
Jason Silva
40mg of cetirizine? Bro, I tried that and felt like a zombie. 😴 But then I switched to fexofenadine + a cold shower every morning and my hives vanished. No pills, no $$$, just science. 🤓🔥
mukesh matav
My cousin in Delhi had chronic hives for years. He stopped all meds, started drinking neem water, and slept on a cotton sheet. No more outbreaks. Maybe the answer isn’t in a pill bottle, but in simple, old ways.
Peggy Adams
Why are we even talking about this? Just don’t eat gluten. Or dairy. Or soy. Or sugar. Or stress. Or breathe. Hives are just your body screaming ‘I hate modern life.’
John Hay
I’ve been on high-dose Zyrtec for a year. Works great. But I stopped cold turkey last month because I was scared of the heart thing. Flared up worse than ever. Back on it now. Just take it. Don’t overthink it.
Stacey Smith
Why are we letting Big Pharma control our health? America needs to ban these drugs and go back to natural healing. We’re not lab rats. #AmericaFirst #StopBigPharma
Sarah Williams
And yet, the only thing that actually works for 70% of people is a drug designed by Big Pharma. Your conspiracy doesn’t change the data. The real villain is the medical system that won’t let patients escalate doses without a fight.
Sarah Williams
Also, Sarah Williams-your comment about the detergent? That’s exactly why tracking matters. I had the same thing. New detergent → flare-up. Switched back → gone. Simple. Not magic. Not conspiracy. Just science.