Understanding Left Ventricular Dysfunction
As a blogger, I often come across various health conditions that impact people from all walks of life. Today, I want to talk about a cardiac condition that is often overlooked in women – left ventricular dysfunction. This condition has unique challenges and considerations that deserve our attention, and I hope this article will help to shed some light on the subject.
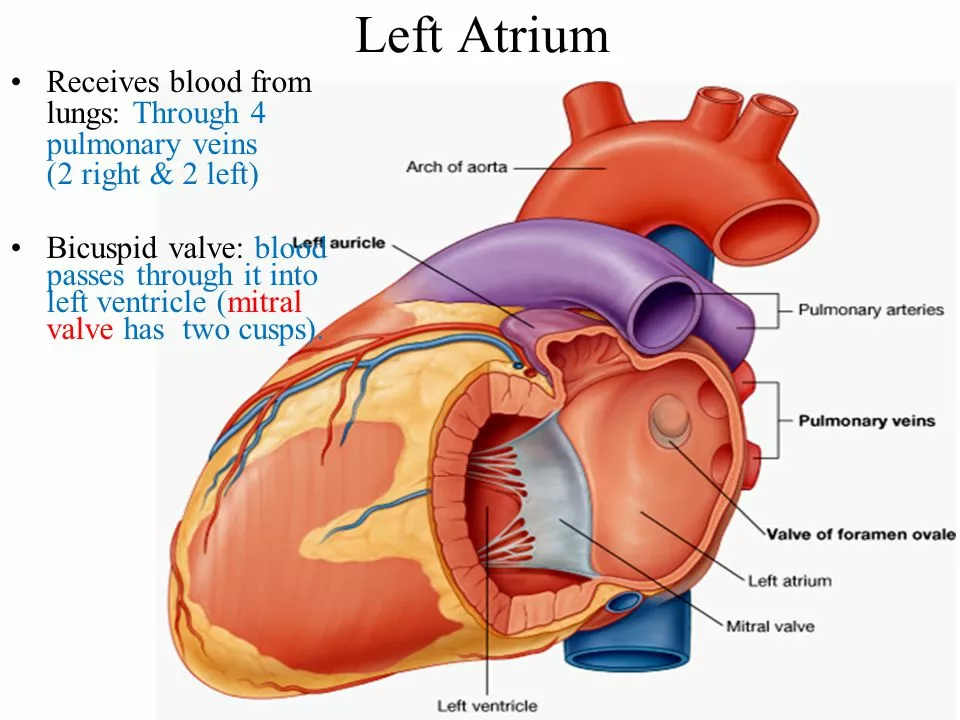
Left ventricular dysfunction refers to a situation where the left ventricle of the heart, which is responsible for pumping oxygenated blood to the rest of the body, is not working efficiently. This can lead to a variety of health problems and complications, particularly for women. Let's dive into the various aspects of this condition and the unique challenges it presents for women.
Signs and Symptoms of Left Ventricular Dysfunction in Women
When it comes to identifying left ventricular dysfunction, it's essential to be aware of the signs and symptoms that may arise. While some symptoms are similar for both men and women, there are some unique manifestations that are more common or specific to women. Some of these symptoms include:
- Fatigue and weakness
- Shortness of breath
- Swelling in the legs and ankles
- Rapid or irregular heartbeat
- Difficulty sleeping, especially when lying flat
- Chest pain or discomfort
- Lightheadedness or fainting
- Decreased exercise tolerance
It's important to note that these symptoms may not always be present or may be subtle in women, making it crucial to listen to your body and seek medical attention if you suspect something is amiss.
Risk Factors and Causes Specific to Women
While left ventricular dysfunction can affect both men and women, there are some risk factors and causes that are specific to women. These include:
- Hormonal changes: Fluctuations in hormone levels during menstruation, pregnancy, and menopause can increase the risk of left ventricular dysfunction in women.
- Pregnancy-related complications: Conditions such as preeclampsia and gestational hypertension can lead to left ventricular dysfunction.
- Autoimmune diseases: Women are more likely to develop autoimmune diseases, which can cause inflammation and damage to the heart muscle.
- Anemia: Women are at a higher risk of developing anemia, which can contribute to the development of left ventricular dysfunction.
- Obesity: Women with obesity are at a higher risk of developing left ventricular dysfunction.
Understanding these risk factors can help women and their healthcare providers make informed decisions about their heart health and take preventive measures when necessary.
Diagnosis and Testing Challenges
Diagnosing left ventricular dysfunction can be challenging, particularly in women. This is because the symptoms can be subtle or mimic other conditions, making it difficult for healthcare providers to pinpoint the cause. Additionally, some diagnostic tests used to detect left ventricular dysfunction may not be as accurate in women as they are in men. Some of the tests that may be performed include:
- Electrocardiogram (ECG)
- Echocardiogram
- Cardiac stress test
- Cardiac magnetic resonance imaging (MRI)
- Blood tests
It's important for women to be proactive about their heart health and discuss any concerns with their healthcare provider, as early diagnosis and intervention can significantly improve outcomes.
Treatment Options for Women
Treating left ventricular dysfunction in women may involve a combination of lifestyle changes, medications, and in some cases, surgical intervention. Some of the treatment options available for women include:
- Medications: Various medications can help improve heart function, reduce symptoms, and prevent complications.
- Lifestyle changes: Adopting a heart-healthy lifestyle including regular exercise, a balanced diet, and stress management can help improve heart function and overall health.
- Cardiac rehabilitation: Participating in a cardiac rehab program can help women learn how to manage their condition and adopt a heart-healthy lifestyle.
- Surgical intervention: In some cases, women may require surgery to address the underlying cause of left ventricular dysfunction, such as valve repair or replacement.
It's crucial for women to work closely with their healthcare providers to develop a personalized treatment plan that addresses their unique needs and challenges.
Prognosis and Long-Term Considerations
With proper diagnosis and treatment, many women can manage left ventricular dysfunction and maintain a good quality of life. However, it's essential to be aware of the long-term considerations and potential complications that may arise. Women with left ventricular dysfunction may be at a higher risk of developing heart failure or experiencing a sudden cardiac event. Regular follow-up care and monitoring are crucial to ensure the condition is being managed effectively and to prevent complications. Additionally, women should discuss their reproductive plans with their healthcare provider, as pregnancy can pose additional risks for women with left ventricular dysfunction.
Emotional and Mental Health Impact
Living with left ventricular dysfunction can take a significant toll on a woman's emotional and mental wellbeing. The physical symptoms and limitations, as well as the uncertainty surrounding the condition, can lead to feelings of anxiety, depression, and stress. It's important for women to seek support from friends, family, and healthcare providers to help them cope with these challenges. Joining a support group, participating in therapy, or engaging in mindfulness practices can also be beneficial in managing the emotional and mental health impact of living with left ventricular dysfunction.
Raising Awareness and Advocacy
As a blogger, I believe it's essential to raise awareness about left ventricular dysfunction in women and the unique challenges and considerations it presents. By discussing this topic openly and sharing information, we can help break down the barriers and misconceptions surrounding women's heart health. Encourage the women in your life to speak up about their heart health and seek medical attention if they notice any concerning symptoms. Together, we can work towards better understanding, diagnosis, and treatment options for women living with left ventricular dysfunction.





Sonia Festa
I swear, every time I feel tired after grocery shopping, I think it's just aging... but now I'm second-guessing everything. My grandma had this weird breathing thing at 62 and no one ever connected it to her heart. We just called it 'getting old.' Maybe we're all just ignoring the signs because it's scary.
Also, why is it always 'women's health' when it's literally a human heart? Why do we keep siloing this?
Sara Allen
I dont get why you guys are so obsessed with this. Men get heart problems too and nobody writes essays about it. Like, my uncle had a triple bypass and no one made a whole blog series about how his heart was 'uniquely challenged' because he was a man. This is just woke medical nonsense. Stop making everything a gender war.
Amina Kmiha
Okay but have you seen the data? 🤔 The FDA has known since 2001 that cardiac tests are calibrated for male physiology. They literally use male heart norms to diagnose women. That’s not negligence - that’s systematic erasure. And don’t even get me started on how pharma trials still exclude pregnant women. This isn’t 'heart disease' - it’s institutional sexism wearing a stethoscope. 💔🩺 #HeartWomensRights
Ryan Tanner
Honestly? This is the kind of content that saves lives. I showed this to my mom after she kept brushing off her fatigue. She went in for an echo and they caught early-stage dysfunction. She’s on meds now and hiking again. You’re not just writing - you’re giving people permission to listen to their bodies. Thank you. 🙌
Jessica Adelle
It is imperative to underscore that the medical community must adhere to evidence-based protocols, not identity-driven narratives. While anecdotal reports may suggest disparities, the peer-reviewed literature remains inconclusive regarding sex-specific diagnostic thresholds. One must not conflate sociopolitical advocacy with clinical science.
Sai Ahmed
They say 'hormonal changes' but nobody talks about how birth control pills and IUDs mess with your endothelial function. And don't get me started on how doctors blame everything on anxiety. I had chest pain for 18 months. Every test was 'normal.' Then I found a cardiologist who actually listened. Coincidence? I think not.
Albert Schueller
The study cited in the link is flawed. They used a small cohort and didn't control for BMI or socioeconomic status. Also, 'autoimmune diseases' - are we sure it's not just the overuse of antibiotics in the 90s? There's a pattern here. I've seen this before. This isn't science - it's narrative-building.
Ted Carr
Ah yes, the classic 'women's heart' article. Next week: 'Men Struggle to Cry Because Society Taught Them to Suppress Emotions.' Groundbreaking. I'll be sure to send this to my cardiologist who also moonlights as a gender studies professor.
Rebecca Parkos
I’m crying. My sister died at 48 from undiagnosed LV dysfunction. They told her it was panic attacks. She was 32 weeks pregnant. I’ve been screaming into the void for years. Thank you for saying this out loud. If one woman reads this and pushes for an echo - it’s worth it. I’m sharing this everywhere.